Removing a Large Flat Colon Polyp by EMR without Surgery
By Jim Sease
Introduction
 An interventional endoscopy doctor at California Pacific Medical Center (Sutter Health) used endoscopic mucosal resection (EMR)
to remove my large flat colon polyp endoscopically without colon surgery. It
was a 5 cm (2 inch) flat sessile villous adenoma colon polyp located in my cecum. All my other
doctors told me I needed laparoscopic right hemicolectomy colon surgery to remove this
polyp. That means they wanted to remove the entire right side of my colon. They said there was no other way. But I had it removed endoscopically by
EMR without colon surgery. Now it's about 15 years later and I still have my entire colon.
An interventional endoscopy doctor at California Pacific Medical Center (Sutter Health) used endoscopic mucosal resection (EMR)
to remove my large flat colon polyp endoscopically without colon surgery. It
was a 5 cm (2 inch) flat sessile villous adenoma colon polyp located in my cecum. All my other
doctors told me I needed laparoscopic right hemicolectomy colon surgery to remove this
polyp. That means they wanted to remove the entire right side of my colon. They said there was no other way. But I had it removed endoscopically by
EMR without colon surgery. Now it's about 15 years later and I still have my entire colon.
My doctors knew about EMR and they knew I really wanted to save my colon, but they did not tell me about EMR. This attitude is far too common. Perhaps this information about EMR will help someone else with a large flat colon polyp who would like to remove it without removing part of the colon. EMR is a safe and effective treatment option for large flat polyps that your gastroenterologist may fail to tell you about.
Endoscopic mucosal resection (EMR) is performed mainly by specially trained and equipped gastroenterologists at certain leading medical institutions who practice interventional endoscopy or therapeutic endoscopy instead of mainstream diagnostic endoscopy. EMR requires advanced endoscopy skills and state of the art endoscopic equipment. It also requires more follow-up care that requires a higher level of skills and equipment. EMR is beyond the capability of most mainstream gastroenterologists so it’s easier for the mainstream gastroenterologist to get rid of your polyp by simply sending you for colon surgery to cut out that part of your colon. They know about EMR and they could refer you to an EMR specialist, but they usually just send you to surgery without telling you about EMR. But who wants to have a large section of colon cut out if they don’t really need to?
This document describes how I found out about endoscopic mucosal resection (EMR), what it is, where to do it, my experience of removing my polyp by EMR, and why it is so important which gastroenterologist and health care organization you go to for colonoscopies, polyp removal, and follow-up care.
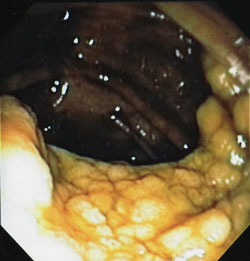
They Found a Colon Polyp and Recommended Colon Surgery
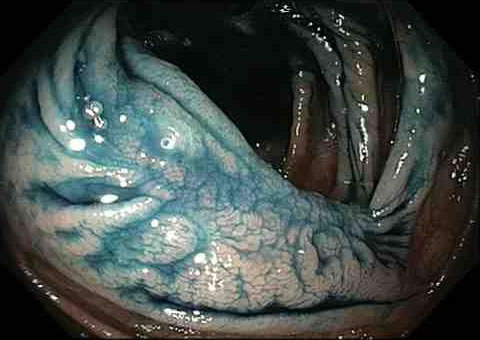
I had a colonoscopy at Kaiser Permanente in July 2007 and they found a very large 5 cm flat sessile villous adenoma colon polyp in my cecum (at the start of the colon near the junction with the small intestine). They could not remove it during the colonoscopy because it was so large and was flat like a carpet against the colon wall and draped over a haustral fold. A colon polyp this large and complicated is sometimes called a giant polyp or a difficult polyp. Fortunately, the biopsy samples were benign villous adenoma.
The polyp is the light colored bumpy looking expanse in the bottom half of the photo shown above. It’s about 2 inches in diameter and a quarter inch thick.
My gastroenterologist told me very briefly as I was coming back to consciousness from the colonoscopy that they found a polyp which needed to be removed. She said fortunately all I needed was laparoscopic surgery instead of full surgery. She said I had an appointment to meet with the surgeon in a couple of days. She made it seem like it was just a small routine procedure to remove the polyp. I thought they would just go in and remove a small little part from my colon where the polyp was located.
I met with the surgeon a couple of days later. He did not have any photos of my polyp or anything yet. I thought how can he know what I need done to my colon without even looking at the colonoscopy photos. He talked about cutting out an 18-inch section of my colon. He made a rough sketch with a pen on a paper with a picture of the colon showing where he was going to remove the entire right side of my colon, part of the transverse colon, the cecum, the ileocecal valve, and large sections of associated blood vessels and lymph system. (Note: The ileocecal valve is a one-way valve at the cecum that has the important function of regulating the flow rate from the small intestine into the colon and preventing backflow from the colon back into the small intestine.) He explained that even though my biopsy samples were benign there was a significant likelihood that my polyp contained cancer anyway. (Note: After my polyp was removed by EMR there was no sign of cancer.) It seemed important to remove all the parts that he was showing me. And since cancer was probably in there, the sooner it was removed the better. He made it seem like it was a fairly urgent situation. He talked about how the recovery would not be all that bad. After a while my bowel habits would probably be fairly normal again. I might have loose bowls and more gas but nothing to be overly concerned about. I questioned the need for such extensive surgery just to remove a polyp. He said the decision about what to remove during the surgery was not his but was the gastroenterologist's decision. He said he could do the surgery the next week. Normally it can take a while to get an appointment for medical treatment, but apparently not for colon surgery. Fortunately, I was having trouble making arrangements for someone to transport me and help me after the surgery so I had to delay surgery. That gave me time to think about it.
The colon is a big part of the body. It's about five feet long and 2.5 inches in diameter. To put this in perspective, a right hemicolectomy removes an amount of the body that is almost as much as your arm. Just like you can get along without your arm, you can get along without a huge section of your colon and the ileocecal valve, but not as well as before. The colon is there for a reason. Also, cutting out large sections of associated blood vessels and lymph system is not without consequences. When they do colon surgery, they cut away the web of connective tissue that connects the colon to the abdominal wall and other organs. Then they pull the colon and part of your small intestine out of your body through a small hole that they cut in your belly. They cut off the 18 inches of colon and the ileocecal valve, staple the small intestine to what’s left of your colon, stuff what is left of your colon back into the hole, and expect it to know how to arrange and reattach itself inside the abdomen. It’s major surgery. In addition to significant loss of functionality, colon surgery is a big hit to the body that takes significant body effort to heal. And I wonder if removing so much of the vital organs could have long-term adverse health effects such as reduced longevity.
Why is it necessary to cut out so much of the colon just to remove a benign polyp? If there were a tumor in your brain or most other parts of your body they certainly would not cut out so much of your body. One of the reasons they cut out so much colon when removing a polyp is that they don't know for sure if the polyp is cancerous or not just from taking a few biopsy samples. What if there is cancer in the part they don't sample? Cancer has a tendency to travel up the blood vessels and lymph system form a cancerous polyp. Surgery is expensive, traumatic, and has some risk of dying, so when they do it, they want to make sure they take out all the necessary parts that might possibly contain cancer so they don’t have to do any more surgery later. So they usually take out an entire block or section of colon, which is served by a system of associated blood vessels and lymph nodes. They don't know the full status of the polyp before surgery because they haven't taken it out of the body yet and can't fully analyze it to see if it really does contain cancer or not.
But what if there was a way to remove the polyp before doing any surgery. Then the polyp could be fully analyzed in pathology and colon surgery would only be necessary in a few cases where they actually do find cancer, since most of the time these benign polyps don't actually have any cancer hidden away inside. So in essence, they could avoid a lot of unnecessary colon surgeries. There is such a method for removing a polyp without doing surgery first. That's what this document is all about.
Over a period of time I consulted with five gastroenterologists and two surgeons about this polyp and they all told me there is no way to heal it and there is no way to remove it except by a right hemicolectomy.
My doctors tried to convince me that colon surgery is no big deal. But it really disturbed me. I know many people feel comfortable with this sort of surgery and would just go ahead and get it done and over with. Or maybe they just don’t think about what they are about to do to the body and simply trust that the doctors know what is best for them. But I could not do that.
Finding an Alternative to Colon Surgery
Instead of having colon surgery, I embarked on a major quest to resolve it in a way that did not cut out part of my colon. The first step was to delay colon surgery so I could fully consider all my options including ones I didn't know about yet and ones that my doctors decided not to tell me about. I soon realized my condition was not a medical emergency. Polyps are normally very slow growing. They can take many years to get as big as mine and my polyp was benign anyway. So why be in a hurry to cut out 18 inches of colon and my ileocecal valve. Once I had the surgery there would be no putting the colon back together again. I rescheduled the surgery several times until finally abandoning the idea of surgery to concentrate on a better solution. I could still get surgery at a later date if necessary.
My doctors had me convinced that my polyp could not be physically removed except by colon surgery so I concentrated on shrinking it or healing it. It’s an interesting story how I tried to shrink it, but I don’t want to distract you from endoscopic mucosal resection, so I won’t go into detail here. But I changed my life style, changed my diet, and went to many alternative health practitioners. I paid out of pocket to get two more colonoscopies to monitor my progress. My polyp did not increase in size and did not turn cancerous while I was trying to shrink it. The main benefit of my efforts was to have enough time to find out about EMR before resorting to colon surgery.
From the beginning, I searched on the Internet for information about polyps. Eventually I discovered endoscopic mucosal resection (EMR) and the removal of large colon polyps. Back in 2007 information about EMR was not as available as it is now. I found the excellent document by Dr. Brian Saunders: “How I Do It” Removing Large or Sessile Colonic Polyps. This was the turning point in my quest to remove my polyp.
What is Endoscopic Mucosal Resection (EMR)?
EMR is a method for removing a large colon polyp with special endoscopic tools and techniques without abdominal incisions or removing a section of the colon. All the work is done inside the colon with endoscopic tools similar to those used in a colonoscopy along with some special attachments and tools that they pass up the colonoscope tube. A saline solution (salt water) is injected into the submucosal layer under the polyp and then the polyp is removed with wires or cutters, either as one piece or in several pieces (piecemeal). The colon wall is protected from damage since the polyp is elevated by the saline solution.
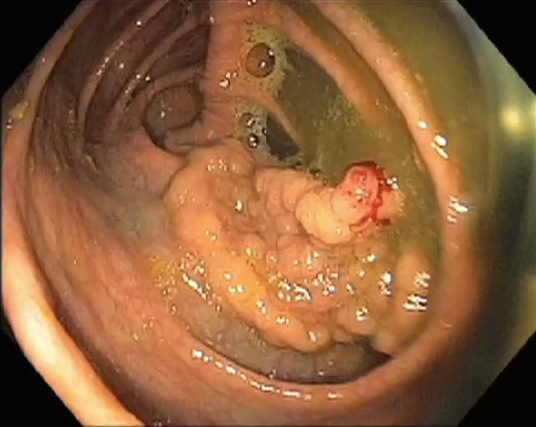
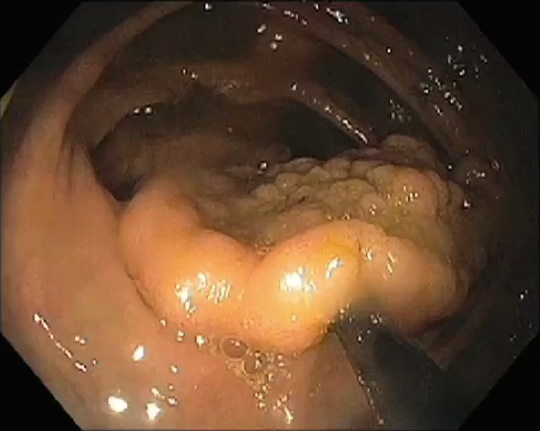
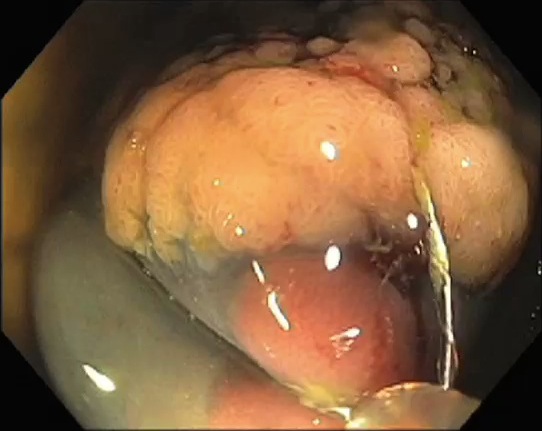
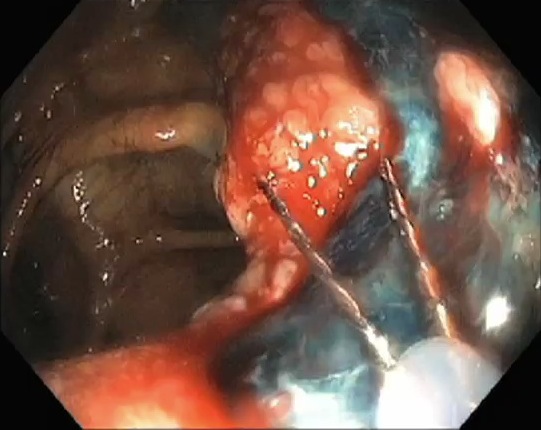
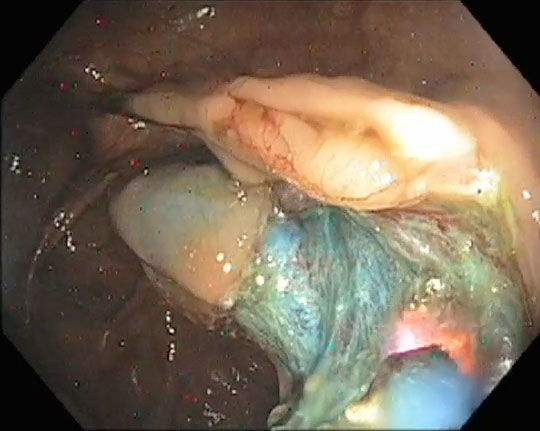
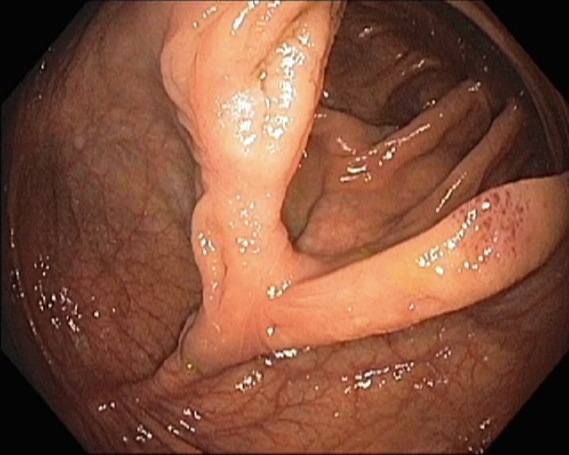
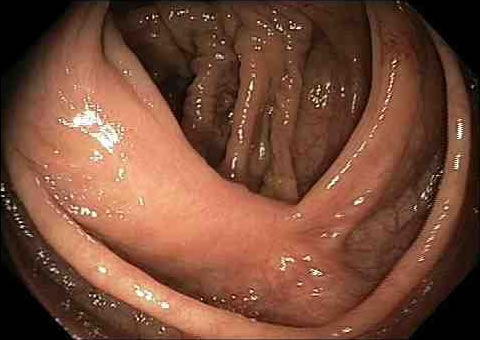
The EMR process is shown briefly in the following photos (left to right).
- The polyp just before EMR.
- The polyp being raised by injecting salt water with blue dye into the submucosal layer under the polyp.
- The polyp being cut with a wire snare which is coming out of the end of the colonoscope tube. The blue color is the salt water injected submucosal layer which is protecting the colon wall from damage during this procedure.
- After the EMR polyp removal. There is still some colored dye showing. The polyp was completely removed down to the colon muscle wall.
- Three months later the colon is completely healed.

It's pretty amazing they can do this. It's all happening five feet up my colon through a colonoscope tube with sophisticated remote digital imaging, remote tools, sophisticated computer technology, and highly skilled operators.
Endoscopic Mucosal Resection (EMR)
This section describes the EMR procedure in more detail.
Initial View
This is the initial view of the polyp, which measures about 5 cm (2 inches) in the longest diameter. The surface pattern of the polyp looks uniform and there is no erosion or ulceration. Endoscopically the polyp is most likely adenomatous (i.e. not cancer).
Injection
Saline (salt water) is injected into the tissue under the polyp to expanded it and raise the polyp from the colon wall. The salt water contains indigo carmine so the solution is tinted with a slight blue color. Thus, we know that as long as there is blue area seen, we are in the correct plane and we don't need to worry about perforation. The wall of the colon is normally only 4 mm thick but is now much thicker with the cushion of salt water. Thus, there is a lot more margin of safety. Plus, the salt water absorbs the heat from the cautery so the cauterization burn does not damage the muscle layers (see the cauterizing step below).
First Cut
This is the first cut using a snare. The first piece of the polyp is removed at its edge.
More Cuts
Numerous additional polyp cuts are performed until the polyp is gone. The blue plane is the submucosa.
Cauterizing Small Blood Vessels
Small blood vessels are cauterized to minimize the chance of bleeding after going home.
Polyp Removed
This is the resected area. The polyp is completely removed.

Three Month Follow-up Colonoscopy
I went back three months after the EMR procedure for a follow-up colonoscopy. The resected site is completely healed.
My Search for an EMR Doctor and Making Arrangements
I knew about EMR but had no idea how or where to have it done or whether anyone could or would remove my particular polyp. I live in Santa Cruz, California, so I searched on the web for someone who could do EMR in Northern California. I looked at names on EMR research papers and also realized that EMR is mostly associated with university medical schools and forward thinking medical organizations. My search led me to California Pacific Medical Center Interventional Endoscopy in San Francisco.
California Pacific Medical Center Interventional Endoscopy is a large state of the art medical services center. They do a wide variety of leading edge interventional endoscopy procedures including EMR. They have a lot of experience with difficult polyps. They have advanced state of the art facilities that go beyond what is normally available to mainstream gastroenterologists. Dr. Kenneth Binmoeller is the CPMC Interventional Endoscopy medical director.
I sent California Pacific Medical Center my colonoscopy reports and a letter explaining my situation. They called and said they could probably remove my polyp. I arranged a special consultation meeting with Dr. Roy Soetikno at California Pacific Medical Center to get more assurance that they could remove my polyp by EMR. Dr. Soetikno said he could not be completely certain from looking at my polyp photos, which were not quite detailed enough, but there was a good chance that he could remove it if there was no cancer growing into the colon wall. He was willing to do the EMR on the basis that he would remove it if possible. It seemed that he had a pretty high confidence level that he could remove it. He told me to see my gastroenterologist and get a referral for EMR.
I went to my gastroenterologist at Kaiser Permanente and asked for a referral for EMR at California Pacific Medical Center. She said she did not recommend it and that I should get colon surgery instead. She really tried to talk me out of it. She knew about EMR all along but she never told me about it. It’s puzzling why she was so opposed to EMR. There are plenty of studies showing that EMR is a safe and effective method for removing large flat polyps like mine. Kaiser did not have any EMR capability at all with their normal in-house staff. They just automatically assume that anyone with a big flat polyp will have it removed with colon surgery. It’s a convenient cozy arrangement. The gastroenterologist simply sends these patients to the surgery department, avoids doing an advanced endoscopic procedure that requires special skills, and avoids doing the post-EMR follow-up colonoscopies, since there is nothing left to check after the surgery. The surgery department is busy cutting out colons and an outside referral to an EMR specialist is avoided. Maybe it fits better with the Kaiser business model to do colon surgery instead of EMR. But what's best for the patient? Most of the time the patient is not even aware that the choice is being made for them to have unnecessary colon surgery instead of EMR. Maybe Kaiser discourages EMR because they know patients would probably prefer EMR instead of unnecessary colon surgery. This way of dealing with large flat polyps is not only at Kaiser but appears to be standard practice throughout most of the medical system.
I pleaded my case for trying to save my colon with EMR. If for some reason EMR didn’t work, I could still do colon surgery later. She reluctantly agreed that if I wanted to do EMR I could. She knew I was a problem patient because I had already been refusing for quite a while to get the recommended colon surgery. I am pretty sure that if I had not been so insistent about wanting to do EMR instead of colon surgery, she would not have requested a referral for EMR. I was determined to get EMR even if I had to pay for it myself. Kaiser did approve the outside referral for EMR at California Pacific Medical Center.
Everything was set. I had a place and time to do it. Kaiser would pay for it. I had a ride with my good friend. All was in order.
Your Search for an EMR Doctor
Finding a doctor for EMR may require some effort. If your gastroenterologist does not refer you for EMR, it's up to you to find a doctor.
When you look for an EMR doctor, you are looking for a gastroenterologist with advanced interventional endoscopy or therapeutic endoscopy skills. You are not looking for a surgeon since EMR is an endoscopic procedure, not a surgical procedure. EMR is basically a normal colonoscopy performed in the gastroenterology department with the use of additional advanced techniques. It normally has nothing to do with the surgery department.
After the gastroenterologist tells you that you have a polyp that requires colon surgery, the next step is usually a meeting with the surgeon to discuss the surgery and to schedule it – usually very soon. It’s common to go looking on the Internet for information before this meeting. You might think, oh I can just ask the surgeon about EMR. But don’t expect much knowledge or enthusiasm about EMR from the surgeon.
Be aware that mainstream gastroenterologists and surgeons often try to discourage you from EMR as being too difficult, risky, impossible, or not appropriate for your particular situation. It can be a mistake to ask your normal gastroenterologist or surgeon about EMR and expect any encouragement. It’s often better to first contact an EMR expert yourself and after that discuss your findings with your gastroenterologist. Typically, the EMR doctor would make an initial determination about your case being appropriate for EMR and then if it seems appropriate would want to see the colonoscopy report or other information for more details. People who are not firm in their resolve could believe their gastroenterologist’s negativity about EMR and not pursue EMR when it could actually work for them. I base these observations on many emails from people reading this web page who pushed through initial discouragement from their gastroenterologist or surgeon and then went on to have their difficult polyp successfully removed by an EMR doctor. One thing to keep in mind is that your gastroenterologist wants to remove that part of your colon anyway, so what’s so bad about trying EMR first. You can still get colon surgery later if necessary.
EMR is highly dependent on the skill of the doctor performing it, so it's important to find a doctor who is good at it, especially if you have an extra difficult polyp to remove. An extra difficult polyp might be something like a very large polyp, a polyp in a difficult location such as touching the ileocecal valve, a polyp that has been subjected to an overly aggressive biopsy procedure, or a polyp that a previous doctor tried to remove by some inappropriate method and failed to remove all of it. These last two items can cause the polyp to not lift when the saline solution is injected under it since scar like tissue has formed. It might take special methods or more work to deal with the polyp or it might not even be possible to remove it. It’s common practice for the initial gastroenterologist to biopsy and tattoo the polyp because they are thinking in terms of colon surgery, not EMR. But this can make the polyp more difficult to remove by EMR. In an ideal world the first gastroenterologist would notice that the polyp can’t be removed by regular methods and leave it alone and refer you to an EMR specialist. But that’s not what usually happens since they are so accustomed to using colon surgery.
I went to Dr. Kenneth Binmoeller at CPMC for a colonoscopy in February 2015. He had some thoughts on this topic: "In skilled hands, virtually any growth that is not invasive cancer can be removed endoscopically. The only time the endoscopist fails is when there is scarring from a prior attempt. With scarring the wall layers become fused and the superficial layers cannot be separated from the deeper. Thus it is important to not attempt resection unless complete removal is likely in one session. If biopsies are obtained, this should be from the edge and kept superficial (not bite-on-bite). India ink injection for tattooing can cause scarring and should be placed a good distance (5 cm) from the lesion and on the opposite wall. The ink spreads along the submucosal plane and can get beneath the growth and cause scarring."
You might think it’s important to find a doctor close to home. It might be possible but it’s not necessarily easy. In the case of EMR, I think probability of success is more important than convenience. You may have only one chance to get the job done right. Good EMR doctors are few and far between. If you are in a hurry it might be best to start by contacting a doctor in the list below and be willing to travel if necessary. If you have some time you could try to find an EMR doctor closer to home.
List of Endoscopic Mucosal Resection (EMR) Doctors
Here is a list of some EMR doctors that I know about. There are many more EMR doctors that are not in this list if you look around.
California Pacific Medical Center (CPMC), San Francisco, CA
Dr. Kenneth Binmoeller performs EMR at CPMC Interventional Endoscopy Center. Dr. Kenneth Binmoeller is the Program Director.
CPMC is where I had my large flat polyp removed by EMR in 2009. Since then I have been to CPMC for four more follow-up colonoscopies.
CPMC is a large state of the art interventional endoscopy medical services center. They have a lot of experience with difficult polyps. There is a collection of Patient Stories written by people who went to CPMC for EMR on Dr. Binmoeller's Endovison website.
During the past few years, Dr. Binmoeller has been using a new method of doing colonoscopies and removing polyps that involves filling the colon with water instead of gas (air/CO2). It's called underwater colonoscopy and underwater EMR (UEMR). Underwater colonoscopy provides enhanced patient comfort, enhanced optics, and other benefits. UEMR eliminates the need to inject fluid under the polyp before removing it. You can learn more about this at Underwater Endoscopy on Vimeo. I experienced this method during my follow-up colonoscopies in 2015 and 2018. I was very impressed. I write more about it later in this document.
Tonya Kaltenbach, M.D. — Palo Alto, Mountain View, and San Francisco, CA
Dr.
Tonya Kaltenbach works at the VA Hospital in Palo Alto. She also does colonoscopy/EMR at El Camino Hospital in Mountain View at 2490 Hospital Drive, Suite 211, El Camino Hospital Campus, Mountain View, CA 94040, phone 650-492-3384, FAX 650-963-3535, advancedgie@icloud.com. She also does EMR procedures at University of California, San Francisco at Mission Bay.
Shai Friedland, M.D. — Stanford Heath Care — Stanford, CA
Dr. Shai Friedland, Stanford Health Care Advanced Endoscopy
Gottumukkala S. Raju, M.D. — Houston, TX
Dr. Gottumukkala S. Raju, MD Anderson Cancer Center in Houston Texas.
Mayo Clinic — Jacksonville, FL
Michael B. Wallace, Mayo Clinic in Jacksonville. The Mayo Clinic considers endoscopic mucosal resection (EMR) as the treatment of choice for large, flat and sessile colorectal lesions (see the article: Endoscopic management of large, flat colorectal polyps).
Mayo Clinic — Rochester, MN
Dr. Louis M. Wong Kee Song, Mayo Clinic in Rochester.
Ian S. Grimm, M.D. — Chapel Hill, NC
Dr. Ian Grimm, UNC, Chapel Hill, NC.
Gregory G. Ginsberg, M.D. — Philadelphia, PA
Dr. Gregory G. Ginsberg, Penn Medicine, Philadelphia, PA.
Jefferson University Complex Colon Polyp Center — Philadelphia, PA
Complex Colon Polyp Center, Jefferson University Hospital, Philadelphia, PA
Sergey Kantsevoy, M.D. — Baltimore, MD
Dr. Sergey Kantsevoy, Director of Therapeutic Endoscopy at Mercy Hospital, Baltimore, MD.
Eric M. Goldberg, M.D. — Baltimore, MD
Dr. Eric Goldberg, Interventional Endoscopy Services, University of Maryland Medical Center, Baltimore, MD.
Mount Sinai Hospital — New York, NY
Mount Sinai Advanced Therapeutic Endoscopy.
University of Chicago Medicine — Chicago, IL
Dr. Uzma Siddiqui, University of Chicago Medicine, Chicago, IL
Read about Dr. Uzma Siddiqui and another web page about her describing EMR Can large colon polyps be removed without surgery?
Northwestern Memorial Hospital — Chicago, IL
Dr. Sri Komanduri, Interventional Endoscopy, Northwestern Memorial Hospital in Chicago, IL.
Douglas K. Rex, M.D. — Indianapolis, IN
Dr. Douglas K. Rex, Indiana University School of Medicine and Indiana University Hospital in Indianapolis.
John Vargo, M.D. — Cleveland, OH
Dr. John Vargo, Cleveland Clinic, Cleveland, OH
Virginia Mason Medical Center — Seattle, WA
Dr. Andrew Ross, Therapeutic Endoscopy Center, Virginia Mason Medical Center, Seattle, WA
John R. Saltzman, M.D. — Boston, MA
Dr. John R. Saltzman, Brigham and Women’s Hospital, 75 Francis Street, Boston, MA
UCLA Health — Los Angeles, CA
Endoscopic mucosal resection (EMR)
University of Colorado Denver — Aurora, CO
Interventional Endoscopy, University of Colorado Denver, Aurora, CO.
Removing the Polyp by Endoscopic Mucosal Resection ó the EMR Procedure
The big day finally arrived in April 2009. I was prepped for the procedure ó no solid food for a day or so, clear liquid diet, GoLYTELY bowel prep, and all the usual stuff for a colonoscopy. The bowel prep and clear liquid diet is a difficult part of EMR and colonoscopies. We got up early and drove to San Francisco.
They took me into the procedure room and got me setup for the colonoscopy. Dr. Roy Soetikno was the doctor. I had an IV in my arm for sedation. They used little or no sedation in the first part when inserting the colonoscope tube. They used light sedation during the EMR. Doctors often use much deeper sedation for EMR than I describe here. I was pretty aware most of the time and remember quite a bit. It was fascinating to watch the EMR procedure on the colonoscopy computer monitors. They had several high-resolution computer monitors in the room. People were moving around but I could see at least one of the monitors most of the time.
I was very impressed with how much skill it took to remove the polyp. It looked like a highly skilled person was playing a high-speed action video game in my colon. I could feel the colonoscope tube moving in and out. The doctor was holding the controller on the end of the colonoscope tube. It looked like a roundish black thing with several control buttons. He was pushing and pulling the colonoscope to position it in my colon. He pressed on the control buttons to control the instruments at the end of the colonoscope tube in my colon. The instruments included things like wire loops, liquid streams, cutting, scraping, fluid injection, and such. I could not feel anything inside my colon where they were removing the polyp. Apparently the colon does not have many nerves for the conscious mind to be aware of. It was sort of like watching a movie. It did not bother me that this was actually taking place in my colon and not just on the computer screen.
At the end of the procedure they gathered all the polyp pieces into a special little mesh basket and pulled them out with the colonoscope tube. It was very satisfying to see the pieces of my polyp being gathered up and taken out in the little basket. I seem to remember them saying they got it all out.
Then I donít remember anything until I woke up in a recovery room. The light was streaming in the windows. It was nice. I was feeling pretty good. I started becoming more aware of where I was. I thought about my friend a couple of blocks away on Fillmore Street shopping and eating at fine restaurants. I found my iPhone and called her. She arrived at the recovery room. It was really good to see her.
I got my EMR report from Dr. Soetikno. The EMR was a success. They got it all out. He gave me a prescription for three days of antibiotics. He said to have a clear liquid diet for two days and then soft food for a couple of days. Watch for bleeding for up to three weeks. Don’t take aspirin or anything that can increase bleeding risk. Come back in three months for a follow-up colonoscopy.
After the Endoscopic Mucosal Resection (EMR) Procedure
We left the hospital and drove home for a couple of hours to Santa Cruz. I was very happy the polyp was gone.
I felt uncomfortable after the EMR procedure. My abdomen was gassy and tender and upset. They pump gas into the colon during the EMR to inflate the colon. Shoving all that endoscopic equipment in and out of my colon and removing a two-inch piece of flesh out of my colon was traumatic to my body even if I didn't consciously feel much.
I was really feeling the adverse effects of eating a liquid diet for a couple days and going most of the day of the procedure with no food or even anything to drink. So on top of the procedure itself, the lack of proper food and water was really affecting me.
For the next few days after the procedure I felt disoriented, uncomfortable, tired, and emotionally delicate. My system was upset due to all the strange diet and trauma from the procedure. I was worried that I might get internal bleeding. There was no way to tell since I was not going to the bathroom yet since I was not eating any solid food and I had been completely cleaned out by the bowel prep before the procedure. I was still on a clear liquid diet for two days after the EMR and I donít feel very good on such a diet. After two days I ate a more normal diet and started feeling better. My digestive system appeared to be working normally. I was relieved that I did not appear to have any bleeding from the EMR procedure.
(Note: Many people have written to me that they felt much less discomfort after the EMR procedure than I describe here. But a few people felt even worse. So I guess it depends on the individual circumstances.)
They took biopsy samples during the EMR procedure and I was waiting for the results. Eventually after several days I got the pathology report. The polyp pieces were villous adenoma (tubulovillous adenoma or villotubular adenoma). That means it was just a polyp and there was no cancer. If there was any cancer it would say something like carcinoma or villous carcinoma. The size of the pieces was 2Ē square and 0.7 cm thick (about 1/4 inch thick). This was good news. If they had found cancer in the polyp, I might need to get colon surgery, although maybe not if it was confined to the polyp and had not gone into the colon wall.
Three Month Follow-up Colonoscopy
I went back to California Pacific Medical Center for the three-month follow-up colonoscopy. Dr. Roy Soetikno was the doctor. The purpose of the follow-up was to make sure the colon healed properly and to remove any remaining or recurrent polyp tissue. The colonoscopy was very straightforward. They used minimal sedation so I was aware of what was going on the entire time. They very carefully examined the site of the polyp with magnification under the following conditions:
- Regular white light
- Narrow band imaging using a green light
- Regular white light with the surface sprayed with a blue dye
The purpose was to compare the pattern of the polyp resection scar area with the surrounding area looking for any irregularities. In my case the pattern was very much the same under all these viewing conditions in both the resection and surrounding areas. This indicates that there was no precancerous lesion. They biopsied the polyp site and confirmed that there was no residual adenoma tissue. The polyp healing process is complete except for more follow-up colonoscopies to check for any new problems.
Following are photos of my polyp resection three months after the EMR procedure.
Viewed with regular white light:
Viewed with narrow band imaging using a green light:

Viewed with regular white light with the surface sprayed with a blue dye:
More Follow-up Colonoscopies
Now that the polyp is gone, what's next? The main issue is that there might be a tiny area of polyp that was not completely removed (residual or remnant) or it might start to grow back (recurrence). It's necessary to get periodic colonoscopies to examine the resected polyp scar area to check for residual/recurrent polyp tissue and remove it while it is small. This is done more frequently at first with longer intervals after the polyp appears to be completely gone. The frequency of colonoscopies depends on various factors and is determined by the gastroenterologist who does each colonoscopy. This may seem like a lot of colonoscopies, but it is normal for anyone who gets a polyp removed by any method to have more frequent colonoscopies.
Nine-Month Follow-up Colonoscopies
It might seem like getting follow-up colonoscopies is straightforward. But there are pitfalls. It's important to get these colonoscopies from gastroenterologists who understand about EMR and are capable of looking for and removing residual/recurrent polyp tissue. Otherwise you could encounter a situation where the gastroenterologist finds a little bit of adenoma tissue and rather than just remove it recommends colon surgery. This would defeat the whole purpose of getting EMR. If this happens you can get another colonoscopy from a properly qualified EMR savvy gastroenterologist to remove it.
This is exactly what happened to me when I went back to Kaiser Permanente for my nine-month follow-up colonoscopy. The Kaiser gastroenterologist found a very tiny bit of adenoma tissue in the EMR scar area and instead of removing it she told me to get a cecectomy (colon surgery to remove my cecum). She showed no intention of supporting me in appropriate post-EMR care. This was quite shocking at the time. I knew she was opposed to me getting EMR in the first place and I intuitively felt she could cause me trouble. But I went to her anyway since that’s what my health insurance provided. This is a good example of why it's important to choose your doctors wisely. After this experience I think it's best to only go to interventional endoscopy specialists for post-EMR colonoscopies and to avoid regular mainstream gastroenterologists unless they clearly have a very favorable attitude toward keeping the colon in one piece.
For the second time with Kaiser I had to take matters into my own hands to avoid unnecessary colon surgery. Without Kaiser's help I went to Dr. Roy Soetikno and Dr. Tonya Kaltenbach for a repeat colonoscopy. They examined my colon very carefully using advanced endoscopic equipment and techniques and they found and removed a very tiny 2 mm area of tubular adenoma residual tissue. Tubular adenoma is the least dangerous type of adenoma tissue. To put the size in perspective, 2 mm is about the size of a pinhead, which is very small. Otherwise the EMR scar area looked healthy and normal. At this point in the follow-ups it is expected to find a situation like this. Remember, the original monster polyp they removed was really large and it was cut off in pieces. It’s expected to find remnants at first. That's why they look for them. My situation was normal.
Two-Year Follow-up Colonoscopy
Dr. Kenneth Binmoeller at CPMC did my two-year follow-up colonoscopy. He inspected the EMR scar area very carefully and found and removed a very tiny 2 mm area of residual tubular adenoma tissue. Otherwise the site looked really good.
Three-Year Follow-up Colonoscopy
Dr. Roy Soetikno did my three-year follow-up colonoscopy in April 2012. He evaluated the EMR scar area very closely using white light, narrow band imaging, and indigo carmine spray. This is the same method for carefully examining the EMR scar that was described in the three-month follow-up section above. No residual polyp tissue was seen. The polyp is completely gone.
Six-Year Follow-up Colonoscopy Using Underwater Colonoscopy
Dr. Kenneth Binmoeller at CPMC did my six-year follow-up colonoscopy in February 2015. There was no sign of abnormal tissue on the EMR scar area. The large flat polyp was completely gone.
This was not a typical colonoscopy. Dr. Binmoeller did it without any sedation using a new technique called underwater colonoscopy that has enhanced patient comfort, enhanced optics, and other benefits. This was an amazing opportunity for me to observe what happens during a colonoscopy. I was fully conscious, and he explained things as the colonoscopy progressed. I had a good view of the computer monitors that he used to perform the colonoscopy. It was very interesting to see the inside of my colon in such detail. During the colonoscopy we discussed this web page as well as the advantages and differences of underwater colonoscopy.
This was my first colonoscopy without sedation. Dr. Binmoeller assured me that an underwater colonoscopy is much more comfortable than a standard colonoscopy using gas (air, C02). During an underwater colonoscopy the colon is lubricated with the water during scope advancement and the colon stays in its natural shape rather than being all puffed up and elongated with gas. This contributes to a more comfortable colonoscopy making it more feasible to do it without sedation. Doing the colonoscopy without sedation was reasonably comfortable. It was uncomfortable when they were advancing it through some of the tight turns. But it was tolerable. Before long they reached the final destination in the cecum. During the rest of the colonoscopy I could feel unusual sensations in my abdomen, but it was tolerable. Any discomfort was more than offset by being fully conscious during the procedure, not needing any recovery time, and not needing an escort to drive me to and from CPMC. At the end of the colonoscopy it only took a little while to get back to my changing area and get discharged since I had not had any sedation. I just got in my car and drove home.
Dr. Binmoeller examined the EMR scar from my previous big polyp. It looked normal. It’s still completely gone. Here is a photo of the EMR scar from a video of my underwater colonoscopy.

Nine-Year Follow-up Colonoscopy Using Underwater Colonoscopy
Dr. Kenneth Binmoeller at CPMC did my nine-year follow-up colonoscopy in July 2018. There was no sign of abnormal tissue on the EMR scar area. The large flat polyp is still completely gone.
Again, this was not a typical colonoscopy. Dr. Binmoeller did it without any sedation using the underwater colonoscopy technique. I was fully conscious, and he explained things as the colonoscopy progressed. I had a good view of the computer monitors that he used to perform the colonoscopy. This is the second time I have had my colonoscopy without sedation using the underwater technique, so I mostly knew what to expect. The sedationless underwater colonoscopy was not completely comfortable. But it was tolerable. I could feel the colonoscope pushing into my colon. Sometimes it got uncomfortable, somewhat like a gas pain, but not exactly. I told him about it and he went more slowly, and it felt better. Any discomfort was more than offset by being fully conscious during the procedure, not needing any recovery time, and not needing an escort to drive me to and from CPMC.
Before long we were at the final destination in the cecum. Dr. Binmoeller examined the EMR scar from of my previous big polyp. It looked normal. It’s still completely gone. He went inside my appendix and also through the ileocecal valve into my ileum (small intestine). In a normal colonoscopy that uses gas, the gas pressure causes these openings to be closed. But underwater these openings tend to be open and receptive. It’s possible for polyps to be in these areas but mine looked normal.
Dr. Binmoeller is interested in the underwater technique for the enhanced ability to detect and remove polyps. He has been perfecting the underwater colonoscopy and UEMR techniques for several years. It has some significant advantages over normal colonoscopies that use gas (air, C02) instead of water in the colon. He uses the water exchange technique which means that as the scope advances in the colon the old less clean water is continuously replaced with fresh clean water. If any residue is noticed it can be washed away. So the colon becomes extremely clean. Another benefit is enhanced optics. In water there is magnification, enhanced surface detail, more natural and intense colors, and a 3-D effect. The very clean colon from the water exchange plus the enhanced optics as well as the fact that lesions tend to float out into the water makes it more likely to notice every little detail resulting in higher adenoma detection rates.
Underwater colonoscopy EMR (UEMR) does not use submucosal injection under a polyp before removing it. This has something to do with the colon wall being in its natural shape and thickness and the fact that lesions tend to float out from the colon wall so it’s easier to get the snare around the lesion to remove it. In addition, the water acts as a protective heat sink which guards against thermal damage from a hot snare. UEMR can be more capable of removing difficult lesions such as scarred and residual lesions as well as lesions involving the appendiceal orifice and ileocecal valve.
Underwater colonoscopy is not available everywhere. I know about it because I happen to go to Dr. Binmoeller and that’s what he does. I know he has made a major effort to utilize and perfect the underwater technique for polyp detection and removal.
I am just touching the surface of underwater colonoscopy and underwater EMR. If you are interested, I recommend looking at Dr. Binmoeller’s website about underwater colonoscopy and underwater EMR (UEMR) at Underwater Endoscopy on Vimeo.
The Large Flat Colon Polyp is Gone
The three-year (2012), six-year (2015), and nine-year (2018) follow-up colonoscopies indicate that there is no trace of abnormal tissue on the EMR scar area. My large 50mm sessile villous adenoma colon polyp is well healed and completely gone.
I should point out that my polyp was more complicated than usual. It's common for polyp removal sites to settle down faster than mine did. My polyp was on a fold, quite large, and removed in several pieces. Other polyps often require fewer follow-up colonoscopies before being completely gone.
I conclude that EMR is an excellent way to remove a large flat polyp. It certainly beats colon surgery. The main downside is that it can be much more complicated to take responsibility for your own health and go outside the normal way of doing things in the medical system. But the upside is that you get to keep your colon.
Background
 I worked for several decades in Silicon Valley (San Francisco Bay Area, California) as an electrical engineer and a technical writer in the semiconductor, electronics, and computer industries. In 2008 when I was figuring out what to do about my polyp I moved from Silicon Valley to Santa Cruz, which is a wonderful seaside resort, a major university town, and one of the main centers of alternative holistic healing in the San Francisco Bay Area. I entered a completely different lifestyle. I parted ways with the Silicon Valley high tech work. I became very involved in holistic health. I mostly focused on shrinking my polyp, alternative health, and enjoying the Santa Cruz lifestyle. It was during this time that I found out about EMR and had my polyp removed without colon surgery.
I worked for several decades in Silicon Valley (San Francisco Bay Area, California) as an electrical engineer and a technical writer in the semiconductor, electronics, and computer industries. In 2008 when I was figuring out what to do about my polyp I moved from Silicon Valley to Santa Cruz, which is a wonderful seaside resort, a major university town, and one of the main centers of alternative holistic healing in the San Francisco Bay Area. I entered a completely different lifestyle. I parted ways with the Silicon Valley high tech work. I became very involved in holistic health. I mostly focused on shrinking my polyp, alternative health, and enjoying the Santa Cruz lifestyle. It was during this time that I found out about EMR and had my polyp removed without colon surgery.
I have a lifelong interest in health, especially alternative health. Both of my parents were very interested in alternative health. I was raised with the idea that the drugs and surgeries that medical doctors offer are not necessarily the best or only approach. Couple this with an unusual aversion to having a big important part of my body cut out and it helps explain my story. The colon is an important part of the body. People often think the function of the colon is to simply suck up excess water and excrete indigestible substances. But the colon does a lot more than that. For example, the colon contains the major portion of the human microbiome, which modern day researchers are finding plays an extremely important role in physical and mental health. This is a super-hot topic in health these days. In my opinion it’s a good idea to keep the colon in one piece if at all possible.
I originally posted this web page in May 2009 shortly after my EMR procedure. This topic was fresh in my mind from spending the previous two years intensively dealing with the polyp. Now it's about 15 years later and thinking about polyps is no longer my top priority. But I realize this web page is still very relevant to some people so I try to keep it up to date. I get colonoscopies, read things, talk to people, and get email from readers of this web page telling me about their experiences with polyps, doctors, and medical procedures. I think about all this and occasionally update this web page.
I made this web page primarily to increase awareness of EMR. I am not qualified to offer medical advice so don’t expect me to tell you what to do about your polyp. Now that you know about EMR and wonder if it applies to you, the most important next step is probably to contact an experienced EMR doctor for a second opinion about your condition. Be aware that if you ask a mainstream gastroenterologist or a surgeon about EMR you are likely to get discouraging answers. It's best to communicate directly with EMR experts if you want to know what they can do for you.
By Jim Sease
jim2045@icloud.com